
Additionally, survival rate of these patients was 94% (17/18), which is significantly higher than previous studies that used SSC and/or dehydration therapy (47% 46/99). We found that plasma brevetoxins declined faster compared to turtles that received only SSC. In total, nine (four subadults, one adult female, four adult males) loggerheads ( Caretta caretta), five (four juvenile, one adult female) Kemp’s ridleys ( Lepidochelys kempii), and four juvenile green turtles ( Chelonia mydas) were included in this study. Blood samples were collected at numerous intervals post-ILE delivery and analyzed for brevetoxins using enzyme-linked immunosorbent assays. Upon admission, blood samples were collected, followed by immediate administration of 25 mg ILE/kg body mass (Intralipid® 20%) at 1 mL/min using infusion pumps.
Sea turtles exhibiting neurological symptoms related to brevetoxicosis were brought to rehabilitation from 2018–2019.

Because red tide events occur annually in Florida, our objective was to test intravenous lipid emulsion (ILE) as a rapid treatment for brevetoxicosis in sea turtles and examine potential impacts on toxin clearance rates, symptom reduction, rehabilitation time, and survival rates.

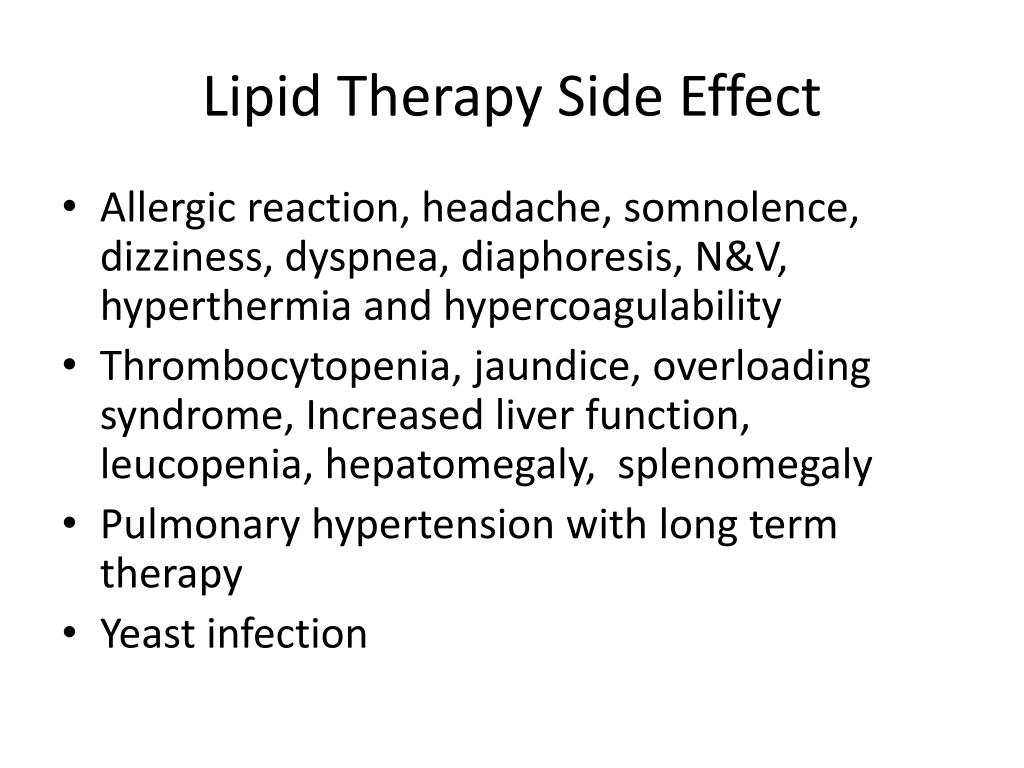
Traditional therapies for brevetoxicosis include standard and supportive care (SSC) and/or dehydration therapy however, these treatments are slow-acting and often ineffective. These dinoflagellates release lipophilic neurotoxins, known as brevetoxins, that bind to sodium channels and inhibit their inactivation, resulting in a variety of symptoms that can lead to mass sea turtle strandings. 2006 Jul 105(1):217-8.The southwest coast of Florida experiences annual red tides, a type of harmful algal bloom that results from high concentrations of Karenia brevis. Rosenblatt M et al Sucsessful use of a 20% lipid emulsion to resucitate a patient after a presumed bupivacaine related cardiac arrest.No evidence to suggest intravenous lipid emulsion used in this context causes pancreatitis. For this reason no definitive answer can be given, only that with the available evidence pancreatitis does not seem to be an adverse affect at this dose. Lipid rescue has not widely been reported on in the literature, only a limited number of case reports exist. The only paper on the subject reports no signs of pancreatitis, although it does not list any specific tests that were carried out. The evidence suggests that pancreatitis is not a risk in the cases in which lipid emulsion has been used in this way. This dictates it may not carry the same risks as when used for total parentral nutrition. When Lipid emulsion is used in the context of lipid rescue it is administered in a very large dose over a short period of time. The follow up period was short only two weeks. It is not stated what evidence for pancreatitis was looked for. Standard resuscitation combined with 100ml 20% Intralipid followed by 0.5ml kg /hr of Intralipid for 2 hours, was successful in reviving. Relevant Paper(s) Author, date and countryĥ6 year old male, 82kg, 170cm who suffered local anaesthetic toxicity while receiving bupivacaine 20ml 0.5% and mepivacaine 20ml 1.5%. AND AND LIMIT to English language and humans. Using Ovid interface Medline 1950 to June week 4 2010, Embase 1980 to 2010 week 26, Cochrane database of systematic reviews 20 In does increase the risk of ? Clinical ScenarioĪ twenty-three year old patient has a number of blood tests carried out within the emergency department, you notice a raised serum amylase, two weeks ago he received lipid emulsion therapy for an accidental local anaesthetic overdose, are these events related?


 0 kommentar(er)
0 kommentar(er)
